A startling investigation into how a cheap, well-known drug became a political football in the midst of a pandemic
August 14, 2020
Early in the coronavirus pandemic, a survey
of the world’s frontline physicians showed hydroxychloroquine to be the
drug they considered the most effective at treating COVID-19 patients.
That was in early April, shortly after a French study showed it was safe
and effective in lowering the virus count, at times in combination with
azithromycin. Next we were told hydroxychloroquine was likely
ineffective, and also dangerous, and that that French study was flawed
and the scientist behind it worthy of mockery. More studies followed,
with contradictory results, and then out came what was hailed by some as
a definitive study of 96,000 patients showing the drug was most
certainly dangerous and ineffective, and indeed that it killed 30% more
people than those who didn’t take it. Within days, that study was retracted, with the editor of one of the two most respected medical journals in the Western world conceding it was “a monumental fraud.” And on it went.
Not
only are lay people confused; professionals are. All that seems certain
is that there is something disturbing going on in our science, and that
if and when the “perfect study” were to ever come along, many won’t
know what to believe.
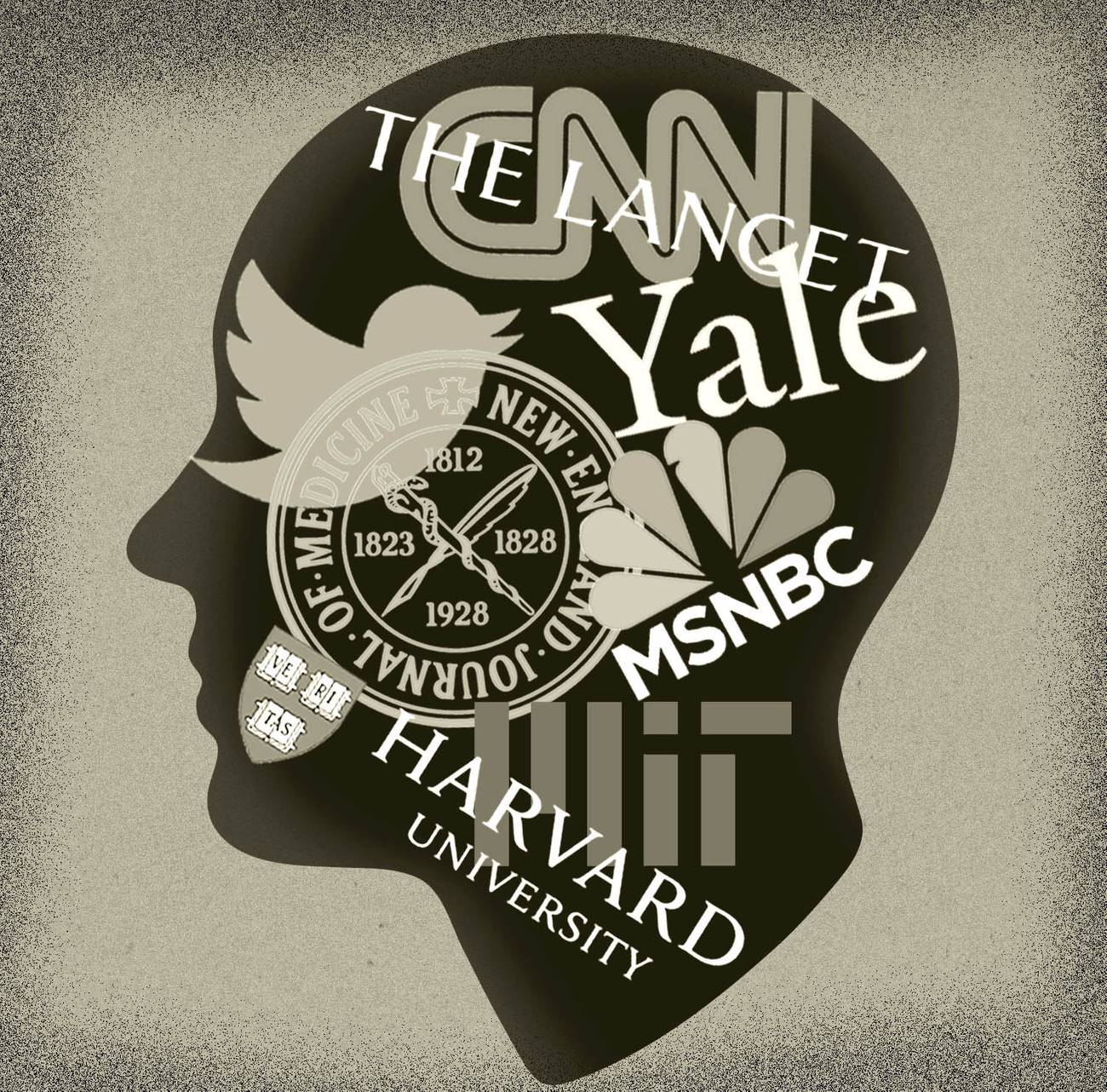
We
live in a culture that has uncritically accepted that every domain of
life is political, and that even things we think are not political are
so, that all human enterprises are merely power struggles, that even the
idea of “truth” is a fantasy, and really a matter of imposing one’s
view on others. For a while, some held out hope that science remained an
exception to this. That scientists would not bring their personal
political biases into their science, and they would not be mobbed if
what they said was unwelcome to one faction or another. But the sordid
2020 drama of hydroxychloroquine—which saw scientists routinely attacked
for critically evaluating evidence and coming to politically
inconvenient conclusions—has, for many, killed those hopes.
Phase
1 of the pandemic saw the near collapse of the credible authority of
much of our public health officialdom at the highest levels, led by the
exposure of the corruption of the World Health Organization.
The crisis was deepened by the numerous reversals on recommendations,
which led to the growing belief that too many officials were
interpreting, bending, or speaking about the science relevant to the
pandemic in a politicized way. Phase 2 is equally dangerous, for it
shows that politicization has started to penetrate the peer review
process, and how studies are reported in scientific journals, and of
course in the press.
Those
who have their doubts about hydroxychloroquine rightly point out that
the public is scared, and we are longing for a magical potion to rescue
us. The history of plagues is rife with such potions and the charlatans
who sold them were well documented in Daniel Defoe’s Journal of a Plague Year. A pandemic is not a remedy for the innate tendency toward wishful thinking.
What
is unique about the hydroxychloroquine discussion is that it is a story
of “unwishful thinking”—to coin a term for the perverse hope that some
good outcome that most sane people would earnestly desire, will never
come to pass. It’s about how, in the midst of a pandemic, thousands
started earnestly hoping—before the science was really in—that a drug,
one that might save lives at a comparatively low cost, would
not actually do so. Reasonably good studies were depicted as sloppy
work, fatally flawed. Many have excelled in making counterfeit bills
that look real, but few have excelled at making real bills look
counterfeit. As such, as we sort this out, we shall observe not only
some “tricks” about how to make bad studies look like good ones, but
also how to make good studies look like bad ones. And why should anyone
facing a pandemic wish to discredit potentially lifesaving
medications? Well, in fact, this ability can come in very handy in this
midst of a plague, when many medications and vaccines are competing to
Save the World—and for the billions of dollars that will go along with
that.
So
this story is twofold. It’s about the discussion that unfolded (and is
still unfolding) around hydroxychloroquine, but if you’re here for a
definitive answer to a narrow question about one specific drug (“does
hydroxychloroquine work?”), you will be disappointed. Because what our
tale is really concerned with is the perilous state of vulnerability of
our scientific discourse, models, and institutions—which is arguably a
much bigger, and more urgent problem, since there are other drugs that
must be tested for safety and effectiveness (most complex illnesses like
COVID-19 often require a group of medications) as well as vaccines,
which would be slated to be given to billions of people. “This
misbegotten episode regarding hydroxychloroquine will be studied by
sociologists of medicine as a classic example of how extra-scientific
factors overrode clear-cut medical evidence,” Yale professor of
epidemiology Harvey A. Risch recently argued. Why not start studying it now?
This
inquiry concerns a molecule that has had so many accusations directed
against it that it now has more than a whiff of scandal. As such, it
might be thought of as a miniature of those eponymous 18th-century
novels of reputation named after a single protagonist, such as Tom
Jones, or Moll Flanders, where the hero’s good name is besmirched early
in life and they must spend the rest of the story hoping to retrieve it.
These adventures are really every bit as much about the societies that
surround the protagonist who, though no angel, has some redeeming
features, and the writer has invented these imperfect, roguish heroes
for the pleasure of seeing them abused and tormented chapter after
chapter, often falsely accused. We are held in suspense, watching the
hero’s rises and falls, waiting to see whether fair play wins out in the
end—or whether he or she is a scoundrel after all, who has pulled the
wool over our eyes. So they are also morality tales.
A
morality tale must have a central character that can arouse some of our
sympathy. When the lead character’s name is the unapproachable and
unpronounceable “C18H26C1N3O,” we are off to a bad start. That it often
goes by “hydroxychloroquine sulfate” doesn’t help. So, like those
English men and women of a certain era with embarrassing names who hid
them behind initials or contemporaries so well known to their audiences
that all one needs are a few letters to recognize them—like FDR or OBL
or DMX—we shall call our protagonist simply: HCQ.
HCQ was first synthesized in 1946,
but came from a distinguished European line. Its esteemed forebear,
“quinine,” made from cinchona bark, had been used to treat malaria
since at least the 1600s. In the 1700s, the Scottish physician and
chemist William Cullen, an important Enlightenment figure, friend of
David Hume, and physician to both Hume and the Scottish king, published
his theory of how quinine cured malaria. Another physician, Cullen’s
near contemporary, Samuel Hahnemann,
translated Cullen’s medical text, and decided to try some quinine
himself, and found it gave him malaria-type symptoms. This so intrigued
him, that it launched him on a new theory of his own—that diseases can
sometimes be cured by substances that, if given to healthy
individuals, give symptoms that are similar to the disease, but if given
to people with the disease, they for some reason get better, such that
“like cures like.” Thereby, homeopathy was born, an approach that
continues to be widely used in Europe and is considered a sign of
insanity by many Western physicians—mature skeptics who prefer to
champion effective and safe medications, like opioids.
For
300 years, quinine, which is not rare—it is in tonic water, for
instance—was the only known remedy for malaria, albeit an imperfect one.
In 1934, German chemists at Bayer synthesized chloroquine in the lab,
and during World War II, that drug was widely used by American forces,
and found more effective than quinine, for both preventing the disease,
and for its treatment. Chloroquine was used widely until the 1960s, when
malaria—Plasmodium falciparum—cleverly had become resistant to
it. But malaria couldn’t resist HCQ, which is nothing but chloroquine
with a slight modification of its chemical structure, an added hydroxyl
group. HCQ was approved for use in 1955, and found to be both more
effective and less toxic than chloroquine, especially when taken for
longer periods. As time passed, both chloroquine and HCQ were found to
be helpful in treating autoimmune diseases like lupus and rheumatoid
arthritis.
Early
in the pandemic, in February and March, I was in Italy, where the death
rate from corona (as it was then called) was astronomical, especially
in the elderly and in frontline medical workers who had sustained
contact with it (in what turned out to be infected hospitals), so I paid
a lot of attention to what the Italian physicians and nurses and
respiratory techs were doing for patients, and to protect themselves.
Stories emerged that often they, and the Chinese frontline physicians
and health care workers, were treating corona patients with HCQ, hoping
it would help, and similarly hoping that by taking it prophylactically,
it would stop them from getting sick. But why?
While
the Chinese Communist Party and government were engaged early in the
pandemic in a well-documented deception of the naive West—withholding
information about the virus, and even banning their physicians from
publishing research on the corona outbreak—behind the scenes many brave
Chinese physicians were nonetheless communicating with Western
colleagues. Wuhan was the epicenter, and the Chinese physicians at the
People’s Hospital of Wuhan University told their Western counterparts
that they got the idea of using HCQ because none
of the 178 patients they had admitted for COVID-19 had lupus—a
surprise, since lupus is an immune disease, and some thought it might
have made these patients especially vulnerable. They wondered why this
might be, and whether HCQ, which these patients had been taking for this
preexisting condition, might in some way be protecting them against
COVID-19.
Even
in an age smitten by the idea that “Big Data Is Our Savior,” many of
medicine’s greatest discoveries begin with precisely these kinds of
chance observations, made by perspicacious frontline physicians looking
at patients, and not from data sets or models, which can often be so
abstract, that they generate only exalted nonsense. The question was:
Could one extrapolate from these few patients—who might have been
protected so far—to others?
A
study in 10 Chinese hospitals was initiated, beginning as early as
January 2020. When they found that 100 Chinese patients did better on
chloroquine than controls, a conference was held on the subject on Feb.
15, in China. The preliminary results were published
as a letter to an English-language journal, claiming they found the
drug was effective against COVID-19-associated pneumonia. Chloroquine
was included in the guidelines for the treatment of COVID-19 issued by
the National Health Commission of the People's Republic of China. By
Feb. 23, seven Chinese studies of chloroquine or HCQ and COVID-19 had
been added to the Chinese Clinical Trial Registry.
There
was another reason studies were necessary. HCQ, though less toxic than
chloroquine, can be dangerous in overdose, and for some people causes
fatal heart arrhythmias, and it can cause retinal problems and blindness
with long-term use (after 10 years of daily use, in 1% of patients),
hearing loss, and even psychosis. Luckily, having been around so long, physicians had come to understand
it very well, knew its dangers, how to screen for the approximately 1%
of people who were vulnerable to these side effects, and also what drugs
it interacted with that might trigger problems (such as
antidepressants). And so, despite all of that, it had been considered
safe enough—if patients were properly screened and monitored by
physicians or trained health care providers, and it was taken in the
right amounts for the proper period of time—to be used throughout the
world. They were still careful: COVID patients were poorly understood
and being administered many new combinations of medications; rather than
just giving HCQ and hoping for the best, scientists began carefully
documenting their observations.
By March, there was evidence from China, published in Nature,
that showed HCQ blocked not only malaria but also the COVID-19 virus in
a test tube. The study showed that HCQ was effective at inhibiting
COVID infections when the scientists put cells (stand-ins for our own)
in culture, in a petri dish, then added the COVID-19 virus, and watched
what happened. Compelling photos
showed how the drug inhibited the development of COVID-19 infections in
the cells, making it a potent “antiviral.” It also decreased
inflammation, which wasn’t that big of a surprise since this property
was the reason HCQ was used to treat autoimmune diseases like lupus and
rheumatoid arthritis, where the body’s inflammatory processes get out of
control and attack its own cells. It was already clear by March that
COVID-19 causes a wild autoimmune response in patients—the “cytokine
storm”—which was often what killed them. But HCQ blocked cytokines, and
moreover, it didn’t damage the cells in the process.
The lab scientists writing in Nature
concluded that HCQ had three things going for it: It seemed safe for
the cells (at least in the short term), was a promising antiviral
against SARS-CoV-2 virus, and an anti-inflammatory compound that had
potential for treating these patients. (It was soon learned that
COVID-19 causes thrombosis or clots, which lead to stroke, and that HCQ
also helped prevent these.)
Then on March 9, there was another Chinese study, published in Clinical Infectious Disease, which showed that HCQ was more effective in inhibiting the COVID virus in the test tube than chloroquine.
Did this mean the drug would cure COVID?
No,
and the study wasn’t designed to demonstrate that. These tests done in
the labs were what are called “proof of concept” studies: Preliminary
studies designed to see if the “concept” that HCQ is an antiviral has
any merit. To prove the drug could cure COVID would require studies in
human beings, which followed patients for significant periods until they
were better, or died, or left with aftereffects of the infection.
Especially influential in much of the world in the early days (if not
the U.S., which often, focuses, it seems, mostly on studies from the
Anglosphere) were studies commissioned by the French government and led
by the microbiologist, physician, and professor of infectious disease
and virology, Didier Raoult,
from l’Institut hospitalo-universitaire (IHU), which he directs in
Marseille, and which had assembled one of the largest datasets in
Europe.
Raoult is the most highly cited microbiologist in Europe, recognized for having identified 468 novel species of bacteria,
most in humans, and for his team having discovered the largest virus
ever documented at the time (so large it had been mistaken for an
intracellular bacterium). He has boldly asserted that viruses—which had
been classified as nonliving—are alive. He has published over 2,000
papers, many of them through the IHU, with him as a contributing or lead
author. He has been given major awards, the French Legion d’honneur,
and perhaps the most important one for a microbiologist, having a
bacteria genus, “Raoutella,” named in his honor.
Raoult
is a fascinating, eccentric, theatrical figure. He couldn’t be more
colorful—a maverick who delights in opposing conventional thinking, his
peers, and followership in science. He has hair to his shoulders, a
long, pointed beard, and looks like a medieval knight in a lab coat. He
loves a fight. At 68 years of age, he rides a Harley to work. He still
treats patients. He sees himself as more like a philosopher or
anthropologist than a typical French scientist, and teaches
epistemology, the study of how we know that we know things, to his lab
scientists, He believes an ever-increasing homogeneity is ruining
scientific thought. He told Paris Match:
I am Nietzschean, I am looking for contradiction, trouble to strengthen myself. The worst is the comfort: It makes you silly ... The more humans you have, the less they think differently. The “politically correct,” the “compliant thinking” are only a mass effect, to be avoided, even if it is difficult to resist! ... To follow the herd no brain is needed, legs are sufficient ... I don’t like movements, I run in the opposite direction. In general, that is where there are nuggets.
As a young man, he was, by his own account a poor student,
and dropped out of school to join the French merchant marine. He
eventually returned to the family trade, conventional medicine, but as
is clear from his work on the interface of bacteria and viruses, the
boundaries drawn by others are not his thing. His frank contempt for
conformity is, not surprisingly, refreshing: He is a kind of Nassim
Taleb of infectious disease. He is brilliant, doesn’t feign false
humility, and claims rather persuasively that he is indifferent to many
of his critics.
Raoult
was the one in his lab who came up with the idea of combining the two
older drugs, HCQ and azithromycin, for COVID-19. A contrarian specialty
of his has been “repurposing” or “repositioning” inexpensive generic and
already available medications to fight infections. Repurposing has huge
advantages. If a drug can be repurposed as an antiviral in an outbreak,
it provides an already approved drug on hand, one with which we have
had years of experience, so we know its drug interactions, how to
monitor its effects on the major organs, how to test for blood levels,
as well as its “posology,” or the science of how a drug’s dosing changes
in different situations, and its safety profile and side effects.
Moreover, old drugs have huge advantages over new ones in this area,
because often bad effects don’t show up for years after the drug is
brought to market. For instance, we now know that methotrexate, which is
used for certain kinds of arthritis, can cause cancer years later;
certain chemotherapies for cancer can cause heart problems
years later. New psychiatric drugs, often heralded to have better side
effect profiles than the current ones on the market, turn out, as time
passes to be far worse, and cause diabetes. The only way to learn about
long term effects of anything is via time.
For many, hydroxychloroquine became viewed as a marker of political identity, on both sides of the political spectrum.
But
drug companies are big businesses, and when they bring a drug to
market, they do studies that display an aptitude for not asking
questions they don’t want the answer to. Relatively little attention is
paid to documenting even short-term side effects in studies. How little?
A recent review
of 192 randomized control trials, in seven different areas of medicine,
showed most randomized control trials for drugs (61%-71%) didn’t deal
adequately with short-term drug toxicity, and those that dealt with it
devoted the same amount of page space, in the published articles, as was
taken up by listing the author’s credentials. And of course we can only
learn of the long-term side effects decades later.
Repurposed
drugs are often generics, and so if one worked during an epidemic, a
society would not have to spend hundreds of millions on developing new
ones, which may or may not work, and may or may not be safe in the long
term. The cost of HCQ for a course of COVID treatment is under $10, and
the cost of another new medication, being evaluated now, remdesivir, is
about $3,500 (which is an entire year’s annual income in some developing
countries, and will not be affordable). So, repurposing also has the
effect of pissing off Big Pharma and those academic courtiers who make
their living from its untold generosity to them.
The
public has almost been trained to think that drugs can only be used for
the purpose for which they are primarily known. People who get cold
viruses and ask their physicians if they can have an antibiotic are told
that old adage: “Antibiotics kill bacteria, not viruses.” And that is
true for most antibiotics. But Raoult’s team was able to show that azithromycin,
classically described as “an antibiotic that fights bacteria,” was
effective in protecting cells that were infected with the Zika virus.
His team also had 20 years of experience of repurposing HCQ for the
long-term treatment of a kind of Q fever—another infectious disease.
Sometimes
drugs developed for noninfectious disease turn out to fight infection.
Some antihypertensives, for example, have antiviral properties, it turns
out. By investigating these relationships systematically—simply
trying old drugs on new conditions and seeing what happened—Raoult was
making a career of, or increasing the probability of, making the kinds
of “chance” observations that the Chinese physicians had made when they
saw that lupus patients on HCQ seemed not to be getting COVID-19. He was
making his luck.
The
idea of studying HCQ as part of a “drug cocktail” to treat COVID-19 had
a personal resonance for Raoult. Part of his childhood was spent in
French Senegal (in Dakar) where his father, a military physician, was
stationed, and as a kid Raoult took chloroquine to prevent malaria. He
had a realistic sense of its long-term side-effect profile, and didn’t
take at all seriously the media characterization of its safer version,
HCQ, as especially dangerous, if taken for several weeks to treat
COVID-19, if patients were properly monitored.
When
the pandemic broke, the first thing that Raoult studied was the effects
of HCQ and azithromycin on “viral load,” or how much COVID-19 virus a
given patient had. Leaving aside other factors—including the patient’s
general health, immune system, diet, Vitamin D status, age, and
more—Chinese physicians knew the amount of virus present correlated with
severity of symptoms
in sick patients, and doctors were beginning to think that “how much
virus” the patient has to deal with was likely a factor in how they
would ultimately fare. The longer that virus had to replicate in the
body, especially in a vulnerable person, the harder it might be to
defeat. So, early in the battle against the virus physicians realized
that if a medication was to work, the earlier it was given to an
infected person the better.
The first small study
by Raoult’s group was begun with 36 COVID-19 patients divided into
three groups: 14 who got HCQ and six who got HCQ and azithromycin for 10
days. (The azithromycin was only added when patients were showing signs
of a lower respiratory tract infection). The third was a control group
of 16 people. These patients were from another hospital that didn’t
offer the new treatment, or people who were offered the treatment but
refused. As we shall see, this approach is very important to Raoult: On
moral grounds he refuses to set up a control group that withholds a
possibly effective treatment from a patient with a lethal illness.
Patients who might be vulnerable to the potential cardiac side effects
were screened and not included in the study, and EKGs were done as
required. It too was a kind of “proof of concept” study, like the
studies of HCQ in the test tube, but taking it to the next level, to see
if the drugs might work to lower the amount of virus in an infected
person’s nasopharynx. COVID-19 was seen as primarily a respiratory
disease at that time, so it made sense to measure the virus there. This
study was answering questions like: Would the drug actually lower the
viral load in the respiratory tract? What would be the appropriate
dose? Would the drugs in combination work synergistically? Lowering
viral load in the nasopharynx alone would not prove that these drugs
would save lives. But without it happening, it would be hard to imagine
saving lives with the drugs would be possible.
The
patients’ noses were swabbed every day, to check for presence of the
virus. By day six, 70% of the HCQ group no longer tested positive for
the virus in the nasopharynx, versus only 12.5% of the control group who
were virus-free. 100% of those who were on both drugs had no virus by
day five. That sounded very good, and seemed to “prove” that the drugs
lower viral load in most patients, in a short time.
Some
criticized the study. While the combination of HCQ and azithromycin’s
effect was dramatic, there were only six patients in that group—not a
big number. Another criticism was that there were six dropouts in the
treatment arm, and they were not included in the final analysis, which
weakened the results. This was not hidden in the paper but discussed and
explained. Studies usually have dropouts. One dropout stopped taking
the medication because of nausea. One person died on day three of
getting the medication. One was transferred to the ICU on the second day
of medication, one on the third day, and one on the fourth day. In
fact, there was nothing original in this discovery of dropouts, since
the authors had pointed them out. These patients had a lethal disease,
and it is not surprising some couldn’t complete the trial. Those who
went to the ICU would then be getting other treatments, which would
confuse the analysis, not clarify it, had they been included.
In
a case of “unwishful thinking,” some people said, in a knee-jerk way,
that the dropouts were obviously a fatal flaw in the study. But, in
fact, the only way to know that would be to check the actual numbers.
Epidemiologist Harry Risch from Yale reanalyzed the raw data—this time
including the dropouts in the analysis. Risch found that their inclusion
“does not much change the 50-fold benefit.”
His analyses also reconfirmed that the drug had to be given earlier in
the illness, to patients with a lower viral load, and that Raoult’s drug
combination did indeed seem to help many patients lower their viral
load.
So:
Those dropouts were not a “fatal flaw” for the study, nor was the
sample size, given its purpose. These “proof of concept studies” are
often small when human beings are involved. Where no effective treatment
exists, you have to start somewhere. And “where” you start—i.e., in
which country or ecology—may also be relevant. Raoult, also an expert in
the history of epidemics, believes that that scholarly discipline
teaches us that ecology—local environmental factors that we don’t
completely understand such as climate, or the presence of other
organisms in a region—influence epidemics, and affect when the peaks
occur and when they recede. Different strains of the coronavirus have
arisen in different parts of the world, for instance. Indeed, sometimes
epidemics do recede, as happened before humanity had medications or
vaccines, again for reasons we don’t totally understand. We also know
genetic factors in different groups can influence differential responses
to medications and perhaps even resistance. Thus it is important to do
studies in different countries, and in different ecological situations.
This was a French beginning, done at the point when there were only
4,500 COVID-19 patients in the country, but already the team had enough
very promising results to be gearing up for the next study of over 1,000
treated patients. A larger and longer follow-up
clinical trial—what is known as an outcome study— would now definitely
be worth the effort, and might show whether lowering the virus in the
nasopharynx correlated with a lasting benefit, such as saving lives, at
least in some patients.
What
the proof of concept study didn’t do was what so many desperate people,
including those in the media who were also personally scared of
COVID-19, wanted it to do: declare that we had a medication combo that
would entirely defeat virus in any and all who were infected. They
wanted a study that would declare that all our troubles were over.
Those
people were skipping steps. In fact, they were skipping science,
because science is about just this kind incrementalism. So here then is a
lesson: When scientific competitors, politicians, and the media, dump
on a study for not showing X, make sure you know whether that study was
even designed with the primary purpose of showing X to begin with.
Raoult’s
clinical group found that for the medications to work, they had to be
given early—something since replicated. This happens with anti-flu drugs
as well—there is a need to stop the virus in its tracks before it
overwhelms the body. This was not only a viral load issue. It had to be
given, it seemed, before the cytokine storms got fully underway.
COVID-19 is almost like two illnesses—one before the storm, and one
after. Any evidence about the use of HCQ and azithromycin given after
the storm starts might well be irrelevant to its effectiveness before
the storm. As well, HCQ is cleared out of the body in significant part
by the kidneys. But the COVID-19 disease process can attack small blood
vessels, and seriously harm the kidneys (and other organs, including the
heart and brain). Basic physiology suggests that giving HCQ after the
kidneys are destroyed would likely mean they would not be able to filter
and clear many of the medications the patients were on, including HCQ,
and so those patients would be more vulnerable to overdose
complications.
Meanwhile,
some American physicians and specialists in infectious disease working
on the frontlines began reporting to American media that they were
seeing HCQ benefits in their own patients too, from some large groups of
physicians at the Henry Ford Health Systems in Detroit, to ones in
private clinics. Two physicians with decades of experience with
epidemics—Drs. Jeff Colyer and Daniel Hinthorn—wrote in the Wall Street Journal, “the
therapy [HCQ plus azithromycin] appears to be making a difference. It
isn’t a silver bullet, but if deployed quickly and strategically the
drug could potentially help bend the pandemic’s ‘hockey stick’
curve.” Given that the American political class and pharmaceutical
industry had outsourced the making of essential medications abroad,
chiefly to China and India, Colyer and Hinthorn publicly asked for
federal help to secure the supply.
Hydroxychloroquine
was not yet a household word. It was just another molecule, making its
way through the world, with a good-enough reputation.
On March 21, President Donald Trump, referring to Raoult’s group’s study (which had appeared just days before), tweeted:
“HYDROXYCHLOROQUINE & AZITHROMYCIN, taken together, have a real
chance to be one of the biggest game-changers in the history of
medicine... Hopefully they will BOTH (H works better with A,
International Journal of Antimicrobial Agents)..... be put in use
IMMEDIATELY...”
A
week later, Trump announced that he was going to make sure that the
United States had a huge stockpile of HCQ. He quickly made a deal with
India—which produced most of the world’s supply, and which had hoped to
keep it for its own citizens—and stockpiled 29 million tablets.
This would make it available for Americans if it turned out it was as
effective as hoped, and also protect supplies for patients with lupus
and rheumatoid arthritis.
Trump
was clearly very excited (and would, according to reports, ultimately
take the drug prophylactically himself), and like many a politician,
wanted to be the bearer of good news in a frightening time. But as so
many had, he slid into seeing Raoult’s very hopeful proof of concept
study as an outcome study.
Let us leave
aside that the biggest game-changer in the history of medicine probably
occurred on the day that physicians and surgeons learned to wash their
hands between patients, and thus stopped killing them while curing them,
and leave aside considerations of how to best convey such information
to a frightened populace as the last few pages show. There was a very
serious line of reasoning, and a case to be made for:
1. Allocating resources to study HCQ and azithromycin in early cases of COVID-19 on a large scale
2.
Making both drugs available on compassionate grounds for an illness
that had no other effective treatment, as was already now routine in
other countries
3. Securing the national supply in case the combo turned out to be as effective as hoped, for COVID-19 patients and for those with lupus and other conditions where it was needed
4. Making clear that the current studies were as of yet small
5.
Making clear these studies were not of HCQ for prophylaxis (studies
that take a lot of time, because the subjects must take the drug and
then be exposed to the virus), but instead that they were of its use in
treating people already infected
Trump’s
political base cheered for HCQ and his opponents booed and accused him
of practicing medicine without a license—and began dredging up any
evidence, or “experts,” they could find, who might emphasize that HCQ
was dangerous, or useless, or both, and thus they responded to his hyperbole with their own, and then some. As Risch observed in Newsweek, for many HCQ became “viewed as a marker of political identity, on both sides of the political spectrum.”
CNN
began a nonstop campaign criticizing the safety of the drug, holding
Trump responsible for three people who overdosed on it in Nigeria.
Rivals went after Raoult, now tainted because Trump had mentioned his
work. A New York Times profile
depicted the scholar-physician as a Trump doppelganger, with his,
“funny hair” and, being a man “who thinks almost everyone else is
stupid,” who “is beloved by the angry and the conspiracy-minded.”
Headlines such as, “Why does Trump call an 86-year-old unproven drug a game-changer against coronavirus?”
were common. Stories began equating HCQ with Trump (“Trump’s drug”) and
emphasized not only that it was dangerous, but that HCQ was old. And
old was definitely not good. The implication was that far better than
old was some new drug—that wasn’t yet invented, never mind tested—that
might be in the utopian “pipeline” to the always better medical future.
What
the media, and public health officials, did not report at the time was
how poor people’s chances were should they go to hospital and need
intensive care for the illness. Hospitals were finding that 80% of
people put on mechanical ventilators died. All the commentators who
railed that HCQ was “unproven” because there had been no randomized
control trials (RCTs) didn’t mention that standard ventilation treatment
for COVID-19, which had become treatment-as-usual overnight for severe
cases, had no RCTs supporting it either. There was a double standard as
far as HCQ was concerned.
Our
poor protagonist, HCQ, could now go nowhere in a hyperpoliticized
America without being hectored and called “Trump’s drug.” In the media,
HCQ was now “touted,” “hyped,” and not “recommended” or “prescribed,” by
the physicians who advocated for it. If someone took the do-it-yourself
approach, as in the sad story of the Arizona man who, terrified out of
his wits of the coronavirus, along with his wife, drank fish tank cleaner
mixed with soda, because she had noticed it had among its ingredients,
“chloroquine phosphate.” His death was blamed on “a chemical that has
been hailed recently by President Trump ...”
This
was all happening at a moment when clinicians working 12- to 15-hour
shifts, seven days a week with COVID patients, probably had more
knowledge of the disease and its treatment than any studies could yet
provide. During this first-wave HCQ-chastisement by the American media, a survey study of 6,200 frontline physicians
in 30 countries showed that, worldwide, HCQ was chosen by the
physicians, from among 15 options, as what they thought was the most
effective treatment for patients (37% chose HCQ). The other drug the
physicians thought highly of was azithromycin.
But
in the United States, HCQ was embroiled in the Republican-Democratic
rivalry. On March 12, Michigan state Rep. Karen Whitsett, a Democrat
representing the 9th Michigan House District in Detroit, went into
quarantine for cornavirus symptoms, and by March 31 got her test results
and was diagnosed with such a serious case of COVID-19 that she thought
she was dying. She and her physician, Dr. Mohammed Arsiwala, sought
permission to use HCQ but could not get it, because the Michigan
Department of Licensing and Regulatory Affairs, under Democratic Gov.
Gretchen Whitmer, had issued an order prohibiting the use of HCQ for
COVID-19.
What
an interesting twist: Plagues always give rise to new customs,
practices, and regulations. If the state can give a medication to some
poor decent citizen on compassionate grounds, indeed why can’t it withhold it on vindictive grounds from a traitor and a fool (as someone who wanted the Trump drug must obviously be)?
Karen Whitsett didn’t feel like assenting to this new reality. Her physician got his hands on some and dared to put her on it. After she recovered, in early April, she thanked President Trump
for having spoken out about the drug, and visited him at the White
House to look into ways it might be made available for others.
In
response, her Michigan Democratic colleagues voted unanimously to
censure her, the resolution stating she had “misrepresented the needs
and priorities” of the Michigan Democratic leadership to the president
and public “in contradiction with the scientifically based and
action-oriented response” of themselves—i.e., the Michigan
leadership—thereby “endangering the health, safety and welfare of her
constituents, the city of Detroit, and the state of Michigan.”
On
April 9, Dr. Raoult’s French center released the initial abstract
reporting their team had now put 1,061 patients on HCQ (for 10 days) and
azithromycin (for five days), and it was ultimately published in Travel Medicine and Infectious Disease
on May 1. All the patients had had viral tests, to establish the
diagnosis, and had electrocardiograms. Genetic analysis of their viruses
was also performed. By publication time 91.7% of those patients had a
good clinical outcome and a virological cure. Eight patients (0.75%)
died, ranging from 74-90 years of age, often having several other
complicating illnesses. These were far better results than in most
centers. They also found that only 5% of the patients were shedding the
virus after the first week of treatment. They reported that none of the
patients had the dreaded cardiac side effects that were being discussed
by some.
Was
this the last word on HCQ? No. According to Raoult’s own scholarly
interest in how epidemics are expressed differently in different
locales, other studies would have to be done. For instance, in
Marseille, Raoult found hardly any obesity in his study population. But
in America, the COVID-19 epidemic was happening on top of another
epidemic: According to the CDC,
71.6% of American adults are overweight, and 39.8% are overweight to
the point of being obese; and obesity, often associated with diabetes,
are two huge risks factors for COVID-19. They might somehow lower the
drug’s effectiveness. One couldn’t assume that because a study showed
the drugs worked in Marseille, they would work in the United States. By
the same token, just because an American study might get poor results
for the combo, wouldn’t mean the Marseille study was inaccurate.
This
study also wasn’t a randomized control trial, intentionally. As noted,
Raoult doesn’t believe in them during a pandemic (nor at some other
times). As he told the Times: “We’re not going to tell someone, ‘Listen, today’s not your lucky day, you’re getting the placebo, you’re going to be dying.”
What
was emerging in scientific circles now was a debate about
“methodology,” or what kind of scientific study of HCQ was appropriate
in an emerging, lethal pandemic.
We
tend to think of methodology as a dry question that has nothing to do
with morality. The methodologist asks what is the best technique to get
at the most certainty most quickly, and usually answers: a randomized
control trial, or RCT. But in medicine, moral concerns can’t be humanely
divorced from methodology. Early in a pandemic, when we know little,
there is a moral imperative to start gathering data. While RCTs are
often (but not always, see below) the best kind of study, they take more
time, and involve randomly assigning, say, half the patients to a new
unknown but promising treatment, and half to either a placebo (sugar
pill) or treatment-as-usual (which might be nothing). They are a type of
experiment. With a milder disease, slow to overtake its victims, with
some viable treatments to compare, one would perform RCTs sooner rather
than later. If the disease is slow to kill, and patients don’t get
better in the study, they might try another treatment or two after the
study ends. But COVID-19 is lethal, kills within weeks when it does, and
there was no good standard treatment for very sick patients, which
meant that in a randomized study, some people would most likely get no
effective treatment, and no second chance with another treatment after
the study was done. Raoult was saying those people were being randomly
assigned to death.
That
is one reason why so many researchers, like Raoult, opted for
observational studies, in which as many patients as possible are
treated. This is not a matter of choosing a design that is “fatally
flawed,” it is a matter of choosing a design that is not unnecessarily
fatal to the patients. It’s is not sloppiness (as some of his critics
would allege), but being true to the study question as he saw it: How
can we save as many lives as possible. These observational studies could
begin almost immediately, and didn’t require the slow approval process
that RCTs require, in part because of the moral dilemmas they raise.
Still,
given that pandemics kill tens of thousands, if not millions, why not
favor the cold-hearted methodologist, who is willing to stand back on a
high hill, like a general in a war, and take some casualties to get a
win sooner? Isn’t that more moral in the long run?
Not
necessarily. It is a common conceit of methodologists that they alone
can improve the quality of medicine, which, without them, would be
hopelessly unscientific. But diseases are very complicated. I know, from
personal experience, that pure methodologists—like “armchair
generals”—i.e., researchers who have perhaps have never treated a single
patient with the relevant illness—often make very elementary errors in
design because they don’t understand how people react to illness, the
illnesses themselves, or the burden of side effects, but rather work
from models. Here is just one kind of such elementary methodological
error. The kind of Russian Roulette RCT I described above, which
involves withholding a possible treatment from a lethal disease, is a
methodologist’s dream design. But you won’t likely volunteer yourself or
loved ones for it if there is a more direct access to a promising
treatment in a dire situation. Almost no sane, nonsuicidal person will,
if properly informed about what is going on (which doesn’t always
happen).
This
is why the role of the “clinician-researcher” developed. A union of
humane medicine with the certitude-seeking scientific researcher, these
people don’t solve all research design problems; rather their role is,
ideally, not to lose sight of the inherent tension of the enterprise.
Anyone who has performed both sides of that compound discipline in good
faith knows there are profound ongoing moral conflicts between the good
doctor, who thinks of the patient in front of him or her, and the
scientist who thinks of the ideal methodology, which—it is hoped—might
benefit other patients in the future. The randomization conflict almost
always exists in serious illness, because we don’t generally study
treatments on dying people that we think have no chance of working. Any
clinician-researcher deserving the name knows that being a researcher
does not cancel out the clinician’s Hippocratic oath to do no harm, or
give them permission not to do what is best for the patient.
So,
how does one sort out what kind of study is appropriate for testing a
new treatment for a lethal disease? Let’s take a little detour to
discuss the models.
Once
a proof of concept study has established that a treatment has a chance
of being effective, then one goes on to do an “outcome study.” Of these,
there are two major kinds: observational studies and randomized control
trials.
The
aim in RCTs, as we’ve said, is to compare those who get that new
medication to those who don’t (or who get another medication). It is
especially important that the two groups are very similar. If the two
groups are very different, it is impossible to tell if the group that
did better did so because of the medication, or perhaps because
of some other characteristic. For instance, we know that advanced age
is a huge risk factor for COVID-19 death. Say one group got the drug,
and the other got placebo, and the group that got the drug had a better
survival rate, but on closer look, was also younger on average. It would
be hard to know if they survived because of the drug or their relative
youth.
Age,
here, is considered a “confounding factor.” It is called a confounding
factor because a naive researcher might think that in the above study,
he or she was measuring “the power of the medication to protect one from
COVID-19 death,” but may actually have also been measuring the role of
youth in protecting the patient from a COVID death. Other confounding
factors we know about now could include how advanced the illness is at
the time of the study, heart disease, diabetes, obesity, or the person’s
vitamin D levels. There could easily be many other confounding factors
we don’t yet know about.
This is where randomization can be very helpful. In a randomized control trial, one takes a large group of patients and randomly
assigns them to either the treatment group, or the nontreatment
“placebo” control group, for instance. It is hoped that by randomly
assigning this large number of patients to either the treatment or
nontreatment condition, that each of the confounding factors will have an equal chance of appearing in both groups.
Observational
studies don’t randomly assign patients to another group. Sometimes they
take people with a chronic illness (which by definition doesn’t
improve) and give them a treatment, and see if they improve. They
compare the patients before the medication and after they got it.
Sometimes they find a control group too. One way they might do so is by
comparing patients in two different settings, where one setting provides
the treatment, and the other setting doesn’t. (This is what Raoult
did). This is a way to get around the moral problem of “withholding”
treatment from the control group—they weren’t going to get it anyway.
Care can (hopefully) be taken to make sure the patients in both groups
are as similar as possible, and are “matched” (say in terms of severity
of illness), but the risk of yet-unknown confounding factors is higher.
For such reasons, many scientists confidently assert that RCTs are
generally better, and many researchers often say—about HCQ for
instance—that we will only know if it works when we get the results of a
large number of large RCTs.
This
implies two things. First, that they are not as confident in the RCT
design sorting out the HCQ problem as they say they are: If the design
is so unshakable and so bias resistant, why would we need to repeat it
many times over? Why wouldn’t one good study be sufficient? Which brings
us to the second implication—namely, that there is safety in numbers:
The more studies show a similar outcome, the more comfortable scientists
will be with it.
Except,
sometimes more studies create more confusion, and are part of a
bandwagon going in the wrong direction. In 2005, Dr. John Iaonnides
published a paper called “Why Most Published Research Findings Are False”
that became the most downloaded paper in the journal PLOS’s history,
and demonstrated that all study designs can, and often do, have
problems—including replication problems, meaning that in a disturbing
number of cases when one group repeats a study or experiment of another
group, they do not get the same findings. He proposed that this was due
to various kinds of bias sneaking in. He also showed there is often a
tendency for a first study to be biased in a certain way, and for that
bias to be picked up and repeated in subsequent studies so that they all
have the same flaw. In this way, a massive library of falsity can build
up, until it is exposed, and overthrown. So, we can’t assume just
because many studies show a particular outcome, that it is true.
One
might think frontline physicians would have protested Ioannides’
findings. But many were not at all surprised, since they too had
witnessed the many reversals of major findings. This is now called the
“replication crisis” in science, or what Nature calls a crisis of “reproducibility,”
and is widely accepted to be a crisis in many fields, but particularly
in the life sciences, psychology, and in medicine—and much less so in
engineering, physics, and astrophysics.
In medicine, it is a problem that is found even in the most respected and cited journals. For instance, a study in The Journal of the American Medical Association
in 2014, also by the Ioannidis group, showed that 35% of the
conclusions of the finest RCTs, assessed by peer review and published in
the most respected medical journals, could not be replicated on reanalysis
of their raw data. Meaning that when researchers gave over their
original data sets to another group, they could not come up with the
same results 35% of the time—in the very best, most-cited journals.
RCTs
are an ingenious tool, a blessed but imperfect gift to humanity, but
the “RCT fundamentalist” is practically a monist, exemplified by the
statement in the text Evidence Based-Medicine: How to Practice and Teach EBM,
which says that when searching for evidence, “If you find the study was
not randomized, we would suggest that you stop reading it and go on to
the next article.”
We now have studies
that show one of the weaknesses of RCTs is that in the quest to
eliminate confounding factors, they end up, in a majority of cases,
excluding patients who are typical of those in the population. The RCT
evangelist focuses only on the RCT strengths, and forgets their
weaknesses. A typical RCT describes several data points about hundreds
of patients. It can be helpful in determining what treatment might work for most people
in a large population. A typical case history describes perhaps
hundreds of data points about a single patient. Its focus might be on
what treatment might work best for this patient. Sometimes we
need all that information about a patient, to choose a proper treatment,
because individual patients differ, often in decisive ways. Patients
are not “several data points.” There are multiple good reasons that the
medical curriculum and major journals and texts publish RCTs,
observational studies, case histories, and other designs, and why most
physicians with experience will use what I would call the
“all-available-evidence” approach and take, as appropriate, what they
can learn from different kinds of studies, and of course everything they
know about their own patient in front of them, to decide on a
treatment. That is what personalized medicine is about. RCT
fundamentalists—who believe only in their randomized data and
essentially argue for throwing away everything else—pose as people
simply expressing the conventional view: All you need is one tool. But
in practice, they are way outside it.
When the teacher tells you to quit paying so much attention to the
fullness of your experience, pay more attention to why he might be
saying so.
For more on the controversy around “Randomized Control Trials,” why “RCT” shouldn’t mean “rigidly constrained thinking,” and on the strengths and weaknesses of different types of studies, see Medicine’s Fundamentalists.
Back
to the world of plague and our poor protagonist, HCQ, who was about to
undergo some extraordinary new trials and adventures in humiliation.
On April 21, the American Veteran’s Administration released a study,
funded by the National Institutes of Health. The authors pointed out
that this was not a randomized clinical trial, there was not a “group
matched design,” and it was not peer reviewed. It was a retrospective
analysis of patients who did and did not get HCQ, in all U.S. Veterans
medical centers until April. It was very reasonable for a large system
to release the best available data they had at the moment, until other
kinds of studies, including RCTs and careful observational studies,
might be released. They reported that 158 patients got standard
management (neither HCL or azithromycin), 97 patients received HCQ, and
113 patients received a combo of HCQ and azithromycin. They followed
these patients and found that of those who got standard care, 11% died,
of those who got HCQ, 28% died, and of those who got HCQ and
azithromycin, 22% died.
In
other words, one would be forgiven for thinking that the people who got
HCQ were much more likely to die, according to this study—if the groups
that got HCQ and those who didn’t were similar.
The
left-leaning media now took up cheering remdesivir the way the
right-leaning media had taken up bashing HCQ. America, I always say, is a
team sport.
But wait: “[H]ydroxychloroquine, with or without azithromycin, was more likely to be prescribed to patients with more severe disease,
as assessed by baseline ventilatory status and metabolic and
hematologic parameters,” wrote the authors (emphasis is mine). The point
should be clear: The HCQ patients were sicker and were more likely to
get the drug as a last resort—just the thing Raoult had warned against.
It was given too late to work.
The
authors had a mathematical way of trying to correct for the problem
that the two groups were not matched on severity by accounting for some
confounding factors after the fact, but ultimately they admitted that
they may have missed some key ones. Though the study didn’t document
cardiotoxicity in the patients, they nonetheless speculated that the
increased cause of death might be related to cardiac toxicity (and not,
for instance, advanced COVID). How did they justify the speculation?
Because a study of chloroquine had found this problem. But chloroquine
and HCQ are different drugs. It was guilt by association.
CNN pounced, and its correspondents and announcers shared the same message. Anderson Cooper
framed it this way: “The President had been out there touting
hydroxychloroquine saying, ‘What do you have to lose?’” The question was
answered by the headline crawler running underneath him: “No Benefits,
Higher Death Rate.” What you have to lose is your life, the network
warned its millions of viewers.
Now
Raoult pounced, and pointed out that there were also objective blood
measures in the study tables, that the authors had not commented on,
showing that those who got HCQ were much sicker than those who
didn’t. Early on, physicians realized that a patient’s white blood cell
count could indicate how close they are to death, as a study eventually published in Nature
made clear. White blood cells are the soldiers in our immune system. As
their numbers collapse, late in COVID, the person’s chances of dying
are vastly increased, meaning that a low white cell count (called
lymphopenia) correlates with a high fatality rate. The reason
for this is being sorted out now; one possibility is those white cells,
or their supportive organs, become infected with the COVID virus and
die. Raoult noted that the pathologically low white count was twice as common in the patients who were given HCQ, so they were much closer to death.
This had not been sufficiently taken into account in the severity
ratings of patients. Secretary of Veteran Affairs Robert Wilke made it clear
that the study “was done on a small number of veterans, sadly those of
whom were in the last stages of life, and the drug was given to them. We
know that the drug has been working on middle aged and younger veterans
... In stopping the progression of the disease.”
He also pointed out that a number of the patients who got HCQ and azithromycin were given the medications after
they had been intubated, so mostly after the cytokine storm had begun,
when organs throughout the body were often already destroyed—way too
late to be effective. Of course it would now tie HCQ into death—and
could be used to falsely suggest those patients were harmed by HCQ, and
not their illness. Raoult also pointed out that the so-called untreated
group had at times received azithromycin in 30% of the cases, so it was
really a “treated” group.
This
same limitation—conducting a study where doctors were more likely to
give HCQ to sicker patients and then comparing how they did with the
less sick group that didn’t get it—would be repeated in several studies
over the next months.
You’ve
heard of cherry-picking evidence or results, when advocating for an
argument, or product or invention. What followed was a torrent of what
could best be called “rotten cherry picking”—media, politicos, and
rivals, scouring the internet for any sign that HCZ would kill masses of
people. For instance, on the same Anderson Cooper show
mentioned above, Dr. Sanjay Gupta listed only the studies that
supposedly showed HCQ didn’t work, and none of the studies that showed
it did.
“A lot of people have gone crazy,” says Raoult,
“claiming that we were dealing with the most dangerous drug in the
world, when almost 2 billion people have already taken it.” HCQ, he
points out, has been given safely for decades, even to pregnant women,
but is being made to look dangerous—even when properly monitored by
cardiologists. In a study,
his team wrote, “There have probably been more than a billion
azithromycin prescriptions around the world since it was first
discovered. The toxicity of each of these two drugs does not, therefore,
pose a major problem. Their possible toxicity in combination has been
suggested in a few anecdotal reports but, to our knowledge, has never
been demonstrated.” As he said in an interview, “It is bizarre, but it is part
of something, you know, that people are completely turned mad about one
of the medics [sic] that have been most prescribed medications in the
history of humanity.”
Meanwhile,
interest was growing in another drug, remdesivir, that had been
developed for Ebola. Dr. Anthony Fauci, head of the U.S. National
Institute of Allergy and Infectious Diseases was enthusiastic—unlike as
he was with HCQ. Even though the early study showed modest gains, Fauci said
“the data show that remdesivir has a clear-cut significant positive
effect in diminishing the time of recovery. This is really quite
important.” The study had shown that those on remdesivir had a mortality
rate of 8.0% vs. 11.6% mortality in the placebo group—statistically
significant, more than a glimmer of hope, less than a cure-all.
Additionally, a not widely reported study
leaked by WHO by accident, showed that remdesivir had no benefits and
that it caused serious side effects to some. But, nonetheless, the
left-leaning media now took up cheering remdesivir the way the
right-leaning media had taken up cheering HCQ. America, I always say, is
a team sport, and each team needs its mascot—or in this case, its med.
On
May 1, the NIH’s COVID-19 Treatment Guidelines panel members allowed
for the emergency use of remdesivir and started pulling away from HCQ,
saying it could only be used in hospital or in studies. Investigative
journalist Sharyl Attkisson looked into the financial links of the
members of that group that was suddenly restricting HCQ and giving the
edge to remdesivir. When she and her team examined the ties of those on
the committee, she found
that a large number had ties with Gilead, the company that makes
remdesivir, which costs $3,500 for several days' worth, and was emerging
as the chief rival to HCQ. It was not just a few members either: “We
found that of 11 members reporting links to a drug company, nine of them
named relationships to remdesivir’s maker Gilead. Seven more, including
two of the committee’s leaders, have ties to Gilead beyond the 11
months they had to disclose. Two were on Gilead’s advisory board. Others
were paid consultants or received research support and honoraria.
Nobody reported ties to hydroxychloroquine, which is now made by
numerous generic manufacturers and is so cheap, analysts say even a
spike in sales would not be a financial driver for the companies.”
Attkisson’s
team also found that one of the authors of the VA study that claimed
HCQ caused increased deaths had received research funding from Gilead,
“including a $247,000 grant in 2018.”
One didn’t have to be an expert in
medical research, or chemistry, to ascertain that the opposition to HCQ
at times was confused and contradictory. Those who opposed it often
gave as their first reason for opposition that “we can’t have
people using HCQ for COVID-19 because we need to keep supplies for
people with rheumatoid arthritis and lupus, who are dependent upon it,”
but adding, sometimes in the same breath, “besides, the drug is a
dangerous killer.”
This
was reminiscent of the initial media messaging around masks, which were
said both to not work and to be desperately needed by medical
professionals. It was a clear case of “both those things can’t be true,” and yet here was Harvard Medical School cardiologist Haider Warraich in the New York Times:
“The bottom line is that even as we are in the midst of a pandemic with
a climbing death toll, hydroxychloroquine has potentially added to the
body count because of its serious possible side effects—like liver and
kidney damage, heart failure and cardiac arrest—and by creating a
shortage of the drug for patients with lupus, whose disease flares when
they don’t take hydroxychloroquine.”
It’s
worth lingering on Dr. Warraich’s statement. It is subtle. By beginning
with the words “the bottom line” and leading to “body count,” the
sentence’s emotional tone suggests we have established definitive evidence that HCQ, even if
prescribed properly by physicians, screening out or at least carefully
monitoring people with heart problems, is a killer. But on closer
inspection, he hedges on that decisive point, and writes HCQ “has potentially added to the body count,” (i.e., it really isn’t certain), and the side effects of which he speaks, are “serious possible
side effects.” He doesn’t quantify how common these side effects are
compared to how many lives might be saved by the drug—a crucial point in
any cost-benefit analysis. By mixing a compound of two “maybes”
(“potential,” and “possible”), he has nonetheless come up with a far
more definite “bottom line.” The article goes on to plead for more
protections for the public from the FDA, a sentiment with which I
completely agree, given the far greater danger posed by many other
drugs.
Warraich
deserves credit for one fact he did express entirely correctly: There
was indeed a serious shortage of HCQ in the United States that was
threatening supply for people with autoimmune disease. It had to be
addressed. But part of the reason it was so hard to get was because
other countries (including Switzerland, India, Brazil, and Israel, among
others) were using it because their public health officials considered
it safe and promising enough, and so they were buying, protecting, even
hoarding it, and by now there were also reports from all over the world
reaching America that physicians were using it prophylactically for ...
themselves.
Anyway, let’s get back to our story—and the moment things took another dramatic turn.
In
May we got two more publications, this time in the two most respected
medical journals in the Western world, that showed that HCQ and
chloroquine increased the death rate of COVID patients by 30%, and
caused heart problems.
The first study was published in the Lancet, and claimed that HCQ and chloroquine caused cardiac arrhythmias and 30% increased deaths
in COVID-19 patients. The study was supposedly based on data taken from
96,000 patients—quite impressive. The same data set was used, in part,
in the New England Journal of Medicine study,
which reiterated that heart disease was a risk factor for COVID-19
death in hospitals, and that certain medications, like ACE inhibitors,
were not a risk. Neither was a randomized control trial, but those were
huge numbers: The kind of “big data” that American computer-smitten
advocates have been insisting would change health care forever for the
better.
The New York Times declared: “Malaria Drug Taken by Trump Is Tied to Increased Risk of Heart Problems and Death in New Study.”
The article itself was quite balanced, and actually warned readers that
these weren’t RCTs and also that they were observational studies with
limits, but the headline had done its job.
Reaction around the world couldn’t have been swifter. As soon as the Lancet study was published, WHO suspended
its own clinical HCQ trial; the United Kingdom’s regulators suspended
all their studies of HCQ, and even France reversed its policy that had
allowed the use of HCQ. On June 15, the FDA revoked the emergency status
use of HCQ with patients (so, perhaps President Trump’s physician, who
is prescribing it for him, should lose his license too now). It seemed
all over for HCQ. Physicians, like Dr. Jon Giles, a rheumatologist at
Columbia University who had used HCQ safely for years, complained that
his research group could no longer get patient recruits
for their HCQ study because they were had been so frightened, and so
they had to abandon it altogether. The Oxford University study of HCQ in
40,000 people for prophylaxis frontline health workers may never get
completed for the same reason. Once drugs are discussed as dangerous,
the lawyers smell business, then physicians smell the lawyers and back
off using it. Licensing bodies now got excited, too, and made hints that
physician outliers could be accused of malpractice and negligence for
using it. HCQ was having a bad week.
Then
two things happened, one on June 4, and one on July 1. One event
illustrated perfectly much that is wrong with modern medicine, and the
other, pretty much everything that is right with it and worth
preserving.
One would figure that the Lancet and the New England Journal
studies must have been very powerful if they were able to slay all the
other HCQ studies in the cradle—including preempting the much awaited
RCTs—and to so impress the scientists at the world’s major public health
organizations, the FDA, and the science-literate writers at the major
newspapers of record.
But fairly suddenly, the studies were retracted.
The
retraction was set in motion when HCQ researchers around the world
noticed all sorts of problems. And these were problems that the study
authors, who were using a big-data approach, seemed not really aware of.
For example, data, supposedly from Australia, was very different from
what was known about Australia’s COVID-19 numbers. The study also
claimed to include cases from Africa, based on extensive electronic
records, and which had testing using advanced medical equipment, that
were not known to exist in many areas of Africa. I myself have worked in
hospitals in Africa, and the scope and kinds of electronic record
keeping they described seemed unlikely.
Over 100 knowledgeable scientists with relevant expertise then signed a letter to the Lancet highlighting the irregularities. In it, they asked the Lancet to have the authors share their raw data.
In
response, the study authors said sorry, they could not identify the
hospitals from which they got their data, or even name the countries
from which they got it, because, they claimed, it was protected by
confidentiality agreements that prohibited them from doing so. You read
that correctly: The researchers hadn’t seen any of these 96,000
patients, or even gathered data from them; it was supposedly all turned
over to their computers, by other computers, in a magnificent data dump.
It
turned out the study authors—the first author was Dr. Mandeep R. Mehra,
of Harvard (that old place again!)—had got their data holus-bolus from
an organization called Surgisphere, which, alas, could not share it
externally. But Surgisphere, it turned out, was all about sharing
internally, because it was run by a vascular surgeon named Dr. Sapan
Desai, who happened to be the brother-in-law of another of the study
authors, Dr. Amit Patel, who was himself a tenured professor of cardiac
surgery. Surgisphere had only a few employees, which included a science
fiction writer and an adult model.
Cornered, the three authors, excluding Sapan Desai, wrote to the Lancet
they were very sorry, but they did an internal investigation of
Surgisphere, and discovered that that entity (which one of the authors
had been in charge of) just couldn’t turn over the records to them,
apologized, and requested their paper be withdrawn. They signed it
listing the dozen companies they had been paid by—mostly drug companies
but some medical equipment makers as well— as a sign of good faith and
transparency. The sister study was retracted from The New England Journal of Medicine an hour after the first was pulled from the Lancet.
Richard Horton, editor of the Lancet, did not pull his punches, and it was he who called it a “monumental fraud.” By focusing on the fraud perpetrated against the Lancet,
he deftly deflected attention away from the monumental inadequacy of
the peer review process at the esteemed journal. Consider that
multitalented crew from Surgisphere claimed that they had somehow
gathered data on 96,000 patients from 1,200 hospitals throughout the
world, and would have been expected to check all 96,000 records, and
analyzed all that data, and done all of this almost overnight. Could
anything have been more implausible? Have you ever tried to get your own medical record from your own local hospital in a jiffy?
And,
if you are a physician, have you ever tried to get medical record
systems, from different hospitals, in the same city, to talk to each
other easily?
There
were other oddities. Though the studies claimed HCQ was toxic, they
often didn’t make clear the what doses of HCQ were administered, and
mixed together patients getting low doses of HCQ with high doses. 66% of
doses it discussed were significantly higher than the FDA recommended
dose. How in the world could the study claim that it was HCQ that was
dangerous, and not the physicians who were overdosing the patients? A
study that didn’t exclude these overdoses seemed almost designed to show
HCQ was unsafe. And the studies didn’t adjust for disease severity as a
confounding variable—so it again blurred together patients too sick to
benefit from HCQ with those for whom it was indicated. It blurred
together people who had COVID-19 induced heart problems with those that
might be caused by the medication. And there was also no ethics review.
The sheer cumulative weight of these flaws—whether the data was
fraudulent or not—should have disqualified the study.
So, is HCQ combined with azithromycin dangerous? The better question to ask is: compared to what?
But
it wasn’t. Perhaps because the study came to the “right” conclusion:
HCQ was dangerous. Far be it for Richard Horton to be accused of mixing
politics and medicine—though he wasn’t all that shy about calling Trump’s defunding of WHO “a crime against humanity.” Perhaps even more revealing: The same week the Surgisphere study came across the esteemed Lancet desk, so did the Raoult study of 1,061 actual patients—but that one was refused.
What
was the reaction of those so skeptical of HCQ to this revelation of the
fraud? Not much. I heard colleagues say just because a study showing it
is dangerous and doesn’t work turns out to be a fraud, doesn’t mean it
is safe and effective—which is of course true—but there was not a lot of curiosity about how easy it had been to dupe the two premier medical journals—or
why. Or whether a growing confirmation bias was now sweeping through
the journals, such that the reviewers could not see through ludicrous
exaggerations, and seemed more impressed by techno-computer-fetishism
and big numbers than simple logic.
On July 1, the cheap, eternally unproven drug seemed, finally, to catch a big break. A large peer-reviewed study of 2,541 patients by the Henry Ford Health Center in Detroit was published in the International Journal of Infectious Diseases.
It showed that HCQ lowered mortality in hospitalized COVID-19 patients
by over 50%. This was a very large effect, in line with the robust
findings Raoult was claiming. Luckily, that study managed to get done
between March 10 to May 2—just before the scare tactics about HCQ made
it harder to get hold of and had all but eliminated people’s willingness
to enroll in such inquiries.
The
Henry Ford study of HCQ was very large, and performed in a hospital
system, consisting of six hospitals. Fifty-six percent of participants
were African Americans, who a number of studies had shown were at higher
risk from COVID than other racial groups, for reasons that are still
being analyzed. It was not a randomized control trial, but was superior
to earlier studies that lumped all patients together and didn’t
effectively distinguish how sick different patients were. This study
took into account 19 different risk factors, and illness severity. So,
unlike the earlier VA study, they did a better partial workaround to
make sure that the patients who received medication, and those who
didn’t, had similar severity of illness. They were also able to match
many of the patients in terms of illness severity of their COVID, and
then compare 190 patients who received HCQ, to 190 matched patients that
did not. HCQ gave a mortality hazard ratio decrease of 51% for those
closely matched patients. Overall, treatment with HCQ decreased the
mortality hazard ratio (the risk of death in the defined time period of
the study) by 66%.
In
that health care system, 26.4% of all patients who had COVID-19, and
got the standard treatment but not the study medications, died. Of those
who received HCQ, only 13.5% died. So, HCQ cut the death rate in half.
As of Aug. 12, over
744,649 people have died of COVID, according to Johns Hopkins
University. If this rate held, in other studies, over 350,000 of those
people might be alive. Worldwide it might save a million or more people
before COVID is tamed.
The
Henry Ford study also studied HCQ in combination with azithromycin to
improve outcomes, and it did. It specified all doses, seemed to get them
right, and gave them at the proper time, early, right after admission,
which as we’ve seen, is crucial to precede the cytokine storm. The study
followed the patient’s electrocardiograms (ECGs), and heart status
throughout, checking for any of the alleged cardiac problems, to make
sure the HCQ didn’t cause harm. It found that with early prescription of
HCQ (82% within 24 hours of hospitalization, 91% within 48 hours), the
patients had far fewer cardiac problems than are usually seen
in later stages of COVID. Since this study, multiple studies have come
out showing that HCQ, when properly monitored, is not
associated with increased cardiac fatalities. The authors made the very
sensible point, that it is probably the case that we will have to work
with several drugs to treat this disease, and the combinations will
likely be different for different patients. Imagine.
CNN called it “a surprising study,” then invited experts to tear it apart, mentioning Trump’s tie to HCQ repeatedly. Anthony Fauci told a House subcommittee
dismissively, “That study is a flawed study, and I think anyone who
examines it carefully [will see] is that it is not a randomized
placebo-controlled trial.” He said it, as though the fact it wasn’t an
RCT had been deliberately buried, and had to be unearthed.
One even-handed critique
of the study—rare in this debate—noted both its strengths and its
weaknesses. One weakness was that patients who got HCQ had received
dexamethasone twice as often as the controls. Dexamethasone is a common
steroid (with a lot more side effects than HCQ) that is used when
inflammation gets out of control. It was good medical practice to not
withhold that drug, but it would likely have been a confounding factor.
If one’s only goal is to determine if HCQ and azithromycin are helpful,
this must be considered a study flaw, as Fauci said. But if one’s goal
is to help people survive, a 66% reduced mortality rate is something to
celebrate, even if it means that the cocktail for COVID-19 might involve
three drugs, for a while. But Fauci didn't seem excited about that. A study
published July 29, from Milan, which also tested HCQ and azithromycin
vs. controls, and which eliminated some of the Henry Ford study
weaknesses, got a 66% reduction of risk compared to controls with the
drug combo.
So, is HCQ combined with azithromycin dangerous? The better question to ask is: compared to what?
When
its foes speak of frightening side effects they do so without ever
quantifying how common they are. Risch did though. He found that of 300,000 people with multiple illnesses,
who had been tried on the medication combination worldwide, the number
of cardiac arrhythmias was 47 per 100,000 and the number deaths (the key
figure) was 9 per 100,000. This was at a time when 10,000 Americans
were dying every week from COVID-19. If the drug combo was able to halve
that number of deaths, as the Ford study suggested, it is easy to see
that the relative risks of the medications are small, and the potential
gain astronomical.
It
is one thing for the HCQ skeptics to have challenged the studies that
said it worked, saying they were imperfect and flawed because they were
not RCTs. But what they really needed in order to put the molecule out
of its misery once and for all were some top notch RCTs to show it
didn’t work. That would finish the job. And that is what happened
next. Official opinions began to morph from, “let’s wait for the RCTs to
settle the matter,” to “it’s already been settled by the RCTs.”
When an RCT by Skipper and colleagues was published in the Annals of Internal Medicine, it came with an editorial accompanying, claiming that this study, along with a few others, were now “strong evidence” against HCQ being more effective than placebo in mild COVID-19 patients. The editorial
then argued that the “the sad saga” of HCQ had almost come to an end.
But, then, “almost at an end” wasn’t soon enough, because the editorial
concluded, “It is time to move on from hydroxychloroquine.”
The
author made no mention of the studies that found the HCQ to be
effective and safe—and instead used only the RCTs that he claimed showed
it was ineffective.
One such RCT was done in China and published in the British Medical Journal.
Yet, once again, the patients were given the medication late—on average
16.6 days after the first symptoms. That guaranteed the HCQ wouldn’t
work well: We already knew HCQ was not for late cases. As well, no
azithromycin was given. Despite that, the HCQ group actually gave more symptomatic relief than the non-HCQ group, but it did not do so at a statistically significant level, But the authors wrote that their study was not
definitive proof HCQ didn’t work—“The results of our main prespecified
outcomes are not entirely conclusive, being based on an underpowered
sample size.” This means they didn’t have enough subjects to make
definitive claims. But that didn’t stop the editorialist, and others,
from claiming more than the authors. On top of that, mysteriously,
sentences that had been in the first preprint version that had been
posted online, were removed in the second version. All the removed sentences spoke to the benefits
of HCQ in more rapidly diminishing symptoms. The Raoult group caught
this covering up of significant pro-HCQ evidence. This, arguably, is a
second scandal in a British medical journal in so many weeks.
Interestingly,
the other RCT cited by the editorial as part of the “strong evidence”
that put the nail in the coffin for the usefulness of HCQ for saving
lives, itself had significant problems, if that was the claim being made
for it (the study authors were not making that claim). It was
not a study to see if HCQ saves lives (though it began so, it was
changed mid-course), but to see if it reduces symptoms. No azithromycin
was used. The patients were given the medication for between a third and
half of the days it is normally given in a typical study to see if the
drug saves lives. (They were given the HCQ for five days, when most
studies use it for 10-14 days, and 21 days in severe cases.) The placebo
used, folic acid, may well not be a placebo at all. There is evidence that in certain forms, folic acid actually can be used to diminish COVID-19, by inhibiting the virus.
Additionally, the patients were not seen
by the investigators—their symptoms were assessed by sending email
surveys to subjects asking them how they felt. This is different than
having them assessed in person, as the French group did. Medication was
mailed to the patients, which meant that some likely got it too late for
it to be effective with weekend delays. In addition, one quarter of
patients reported they didn’t take the medication they did get
as prescribed. Almost half the patients did not have a viral test
confirming the diagnosis. This was early in the pandemic, and they were
in short supply at the time in the United States, and had a long
turnaround time. The lack of early rapid testing, and thus quick
diagnosis, also suggests that many patients may have got their
medication too late to be effective. Even so, the HCQ group, despite all
these obstacles, had more diminishment of their symptom severity
compared to the placebo group—i.e., HCQ did better, just not to the
point of being statistically significant. Half as many in the HCQ group
had to be hospitalized. It leaves one wondering how HCQ would have
performed in terms of saving lives (the most important question), if all
the patients who took it did so promptly and actually got a standard
amount, and not half to a third, and were properly monitored to take it
as prescribed. It is one of three RCTs that actually show, in their
results sections, that HCQ did better than placebo, but which
in their conclusions, the authors claim the opposite. This is based on a
confusion about how to draw conclusions from statistics. This error is
clearly explained in an international letter,
signed by medical statisticians and mathematicians who are disturbed by
the use to which these studies are being put, given their actual
results.
The
evidence from these RCTs for the assertions that HCQ, combined with
azithromycin doesn’t work in the early cases is astoundingly weak—looked
at closely, a few of those studies actually are closer to supporting
HCQ. Yet, when Assistant Secretary for Health Admiral Brett Giroir,
M.D., who is also a member of the White House Coronavirus Task force, appeared on Meet the Press
on Aug. 2, he seemed not to know that, or any of the evidence in its
favor. Host Chuck Todd asked the admiral: “I know you’re not a political
person, but the president continues to advocate for hydroxychloroquine,
is that a danger to public health? The admiral replied, parroting the
recent editorial: “I think we need to move on from that ...” He
elaborated, saying: “At this point in time we don’t recommend that
[hydroxychloroquine] as a treatment. There’s no evidence to show that it
is ... Most physicians and prescribers are evidence-based and they are
not influenced by whatever is on Twitter or anything else.”
His
assertion implied that anything that had been said in favor of HCQ was
the product of Twitter and not serious studies; it was a claim tone deaf
to the fact that the clinicians and researchers in whose name this
assertion was made, were some of the very ones who knew of these
positive studies—who, in some cases, were the ones who conducted them, and who still stand by them.
Indeed,
at this point confirmation bias against HCQ has been so intense,
especially among those who don’t have experience prescribing it, that
the bias-holders simply ignore large studies like Ford and brush aside
the fact that the drug had been safe enough to be a standard of care for
decades. They have even ignored studies that are broadly negative,
including an RCT from the United States and Canada combined
that showed that HCQ did not work as a prophylactic to people who had
high risk exposures to COVID-19 contacts, but which also showed that
“there were no serious intervention related adverse reactions or cardiac
arrhythmias.” It has begun to seem like, unless a study justifies a
visceral and comprehensive skepticism for HCQ, it won’t get
attention—let alone be taken seriously. And what does “moving on from
HCQ” even mean? Banning it? Closing down the RCTs that are ongoing? One
thing 'moving on' means is that the FDA is now overriding large
organizations that had access to HCQ, and want that access to continue.
On Aug. 13, it was revealed that the large Henry Ford Hospital System,
based on their study and the requests of their frontline physicians, had
asked the FDA to let them continue using HCQ for their patients, though
the study had ended. The FDA refused.
So
this is likely how it’s going to be. Poor HCQ will remain a kind of
Rorschach inkblot test, saying more about one’s projections than itself.
Or, to switch metaphors, it seems destined to carry an orange T on its
forehead, a warning to sensible people to steer clear.
Lots
and lots of COVID-19 studies will come out—several hundred are in the
works. People will hope more and more accumulating numbers—and more big
data—will settle it. But big data, interpreted by people who have never
treated any of the patients involved can be dangerous, a kind of exalted
nonsense. It’s an old lesson: Quantity is not quality.
On
this, I favor the all-available-evidence approach, which understands
that large studies are important, but also that the medication that
might be best for the largest number of people may not be best one for
an individual patient. In fact, it would be typical of medicine that a
number of different medications will be needed for COVID-19, and that
there will be interactions of some with patient’s existing medications
or conditions, so that the more medications we have to choose from, the
better. We should be giving individual clinicians on the front lines the
usual latitude to take account of their individual patient’s condition,
and preferences, and encourage these physicians to bring to bear
everything they have learned and read (they have been trained to read
studies), and continue to read, but also what they have seen with their
own eyes. Unlike medical bureaucrats or others who issue decrees from
remote places physicians are literally on our front lines—actually
observing the patients in question, and a Hippocratic Oath to serve
them—and not the Lancet or WHO or CNN.
As
contentious as this debate has been, and as urgent as the need for
informed and timely information seems now, the reason to understand what
happened with HCQ is for what it reflects about the social context
within which science is now produced: a landscape overly influenced by
technology and its obsession with big data abstraction over concrete,
tangible human experience; academics who increasingly see all
human activities as “political” power games, and so in good conscience
can now justify inserting their own politics into academic pursuits and
reporting; extraordinarily powerful pharmaceutical companies competing
for hundreds of billions of dollars; politicians competing for
pharmaceutical dollars as well as public adoration—both of which come
these days too much from social media; and the decaying of the
journalistic and scholarly super-layers that used to do much better
holding everyone in this pyramid accountable, but no longer do, or even
can. If you think this year’s controversy is bad, consider that
hydroxychloroquine is given to relatively few people with COVID-19, all
sick, many with nothing to lose. It enters the body, and leaves fairly
quickly, and has been known to us for decades. COVID vaccines, which
advocates will want to be mandatory and given to all people—healthy and
not, young and old—are being rushed past their normal safety precautions
and regulations, and the typical five-to-10-year observation period
is being waived to get “Operation Warp Speed” done as soon as possible.
This is being done with the endorsement of public health officials—the
same ones, in many cases who are saying HCQ is suddenly extremely
dangerous.
Philosophically, and psychologically, it is a fantastic spectacle to behold, a reversal, the magnitude and the chutzpah
of which must inspire awe: a public health establishment, showing
extraordinary risk aversion to medications and treatments that are
extremely well known, and had been used by billions, suddenly throwing
caution to the wind and endorsing the rollout of treatments that are
entirely novel—and about which we literally can’t possibly know
anything, as regards to their long-term effects. Their manufacturers know this well themselves, which is why they have aimed for, insisted on, and have already been granted indemnification—guaranteed,
by those same public health officials and government that they will not
be held legally accountable should their product cause injury.
From
unheard of extremes of caution and “unwishful thinking,” to unheard of
extremes of risk-taking, and recklessly wishful thinking, this double
standard, this about-face, is not happening because this issue of public
safety is really so complex a problem that only our experts can
understand it; it is happening because there is, right now, a much
bigger problem: with our experts, and with the institutions that we had
trusted to help solve our most pressing scientific and medical problems.
Unless these are attended to, HCQ won’t be remembered simply as that
major medical issue that no one could agree on, and which left
overwhelming controversy, confusion, and possibly unnecessary deaths of
tens of thousands in its wake; it will be one of many in a chain of such
disasters.
* Update, Aug. 14: This
article has been updated with new information on the aftermath of the
peer-reviewed HCQ study conducted by the Henry Ford Health System in
Detroit. * Update, Aug. 15: This article originally described a study published in May in the Lancet
that claimed to show COVID patients given the drug HCQ experienced
increased health risks. The article has been updated to reflect that the
study examined both HCQ and the drug chloroquine.
Norman Doidge, a contributing writer for Tablet, is a psychiatrist, psychoanalyst, and author of The Brain That Changes Itself and The Brain’s Way of Healing.